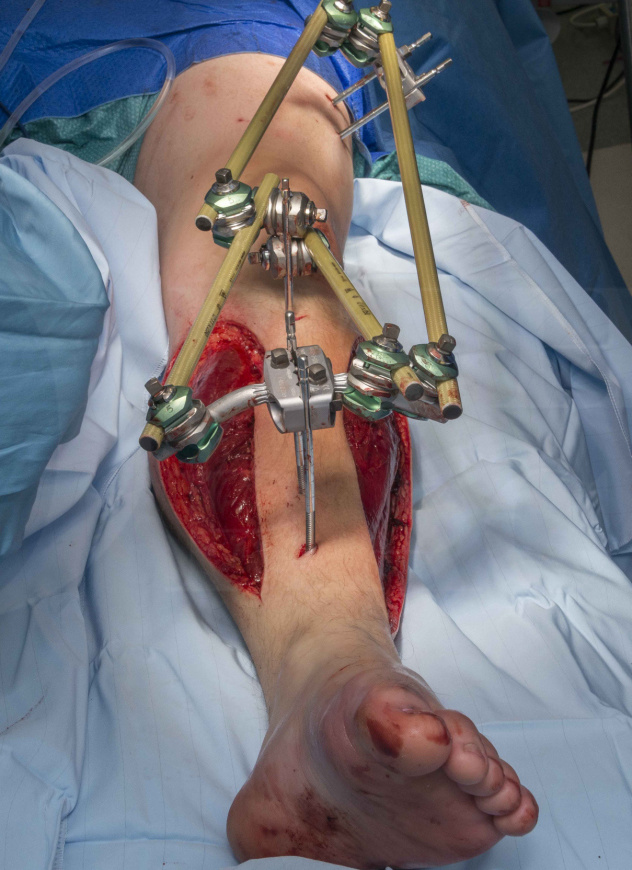
Compartment fasciotomy and Hoffmann 3 spanning external fixator for open tibial fracture
Overview
Subscribe to get full access to this operation and the extensive Knee Surgery Atlas.
Professional Guidelines Included
Learn the Compartment fasciotomy and Hoffmann 3 spanning external fixator for open tibial fracture surgical technique with step by step instructions on OrthOracle. Our e-learning platform contains high resolution images and a certified CME of the Compartment fasciotomy and Hoffmann 3 spanning external fixator for open tibial fracture surgical procedure.
Open fractures of the tibia are the most common open long bone fracture with an annual incidence of 3.4 per 100,000 population. The mean patient age is 43 years however, the distribution is bimodal. They most frequently affect young adult males and elderly females. The usual mechanism is from high energy trauma such as a motor vehicle collision or a fall from significant height.
Open tibial fractures have been classified by Gustilo and Anderson in 1976 and subsequently revised in 1984. The fractures are first classified by the mechanism of injury – energy level. High energy injuries are automatically a type III. Type III is further subdivided into A, B and C.
- Type I: Low energy; wound less than 1cm; clean; simple fracture pattern.
- Type II: Low energy; wound greater than 1cm; soft tissue damage not extensive; no flaps or avulsions; simple fracture pattern.
- Type III: High energy; extensive soft tissue damage; or multi-fragmentary fracture / segmental fracture / bone loss irrespective of soft tissue wound size; or severe crush injury; or vascular injury requiring repair; or severe contamination including farmyard injuries.
Type III has been subdivided into:
- III-A: Adequate soft tissue to cover the bone.
- III-B: Extensive soft tissue injury with periosteal stripping and bone exposure; major wound contamination.
- III-C: Arterial injury requiring repair.
Importantly the Gustilo Anderson classification should only be determined after surgical debridement and must recognise the energy level from the mechanism of injury.
More recently the Ganga Hospital classification system has been developed in an effort to help better prognosticate between limb salvage or amputation. This system scores 3 criteria (skin, soft tissues, and skeletal damage) from 1 to 5 and also has additional risk factors (age > 65; contamination; chronic illness; systemic injury; other trauma – 2 points per additional risk factor). The score correlates with the recommended treatment and likely outcomes. It is most useful for Gustilo Anderson III-B injuries as this is a broad group. It has also shown greater sensitivity and specificity for predicting amputation compared to other severity scores. A score of 14 or less (out of 29) has shown good specificity and sensitivity for recommending limb salvage. A score of 17 or more has shown similar accuracy for predicting amputation.
Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Joint Surg [Am] 1976; 58-A: 453-8.
Rajasekaran S. Ganga hospital open injury severity score – a score to prognosticate limb salvage and outcome measures in type IIIB open tibial fractures. Indian J Orthop 2005; 39: 4-15.
The principles for the management of open fractures have been agreed between the British Orthopaedic Association (BOA) and British Association of Plastic Reconstructive and Aesthetic Surgeons (BAPRAS). Their recommendations are available for download as a standard for trauma (BOAST). Here is a summary of the standards:
- Patient’s with open fractures of long bones should be managed in a specialist centre that can provide combined OrthoPlastic care.
- Antibiotics should be administered ideally within 1 hour of injury.
- The injured limb should have regular / documented assessment of neurovascular status.
- The limb should be realigned and splinted.
- Continuous assessment to avoid compartment syndrome.
- The wound should be photographed and covered with a saline soaked gauze (avoid repeated ‘looking’ and mini-washouts).
- Timing of debridement:
- Immediate – highly contaminated (agriculture, aquatic, sewage) or vascular compromise
- Within 12 hours – for solitary high energy injuries
- Within 24 hours – for all low energy injuries
- Definitive soft tissue cover / closure in 72 hours.
Compartment syndrome is defined as a rise in pressure within a fascial compartment causing local tissue ischaemia and hypoxia. This is manifest by a progressive and deteriorating situation. Initially the interstitial pressure of the compartment rises. This causes the thin-walled veins to collapse thus causing venous hypertension. The blood flow out of the compartment is therefore comprised and like a traffic jam it starts to back up as the arterial inflow pressure is still greater than the compartment pressure. With the onset of cellular death, the cell membranes rupture and release osmotically active cellular contents into the interstitial space. This creates an osmotic gradient which draws more fluid into the compartment and hence increases the pressure further. Myonecrosis can occur within 2 hours of onset of ACS and after 6-8 hours irreversible ischaemic damage has occurred. Eventually the pressure is such that the arterial supply is compromised and clinically this is recognised with absent pulses. This is a late stage and should be avoided at all costs.
In this technique I present the case of an open tibial fracture following a crush injury mechanism. A heavy goods vehicle (HGV) axel fell off a stand and trapped the patient’s limb for a few minutes while co-workers struggled to lift it and extricate the patient. Here prophylactic fasciotomies have been performed, as the likelihood of developing an ACS is high.
The fracture has been temporarily stabilised with the Hoffmann 3 External Fixation system. This is a modular, multi-planar external fixation system with independent pin placement capabilities, rapid assembly Snap-Fit couplings and it’s MRI conditional up to 3.0 Tesla. The Hoffmann 3 was developed for use in acute trauma, damage control orthopaedics and definitive fracture fixation. The Delta Couplings are compatible with Hoffmann II and you can use any combination of 5, 8 and 11mm connecting rods.
Readers will also find the following OrthOracle techniques of use:
Fasciotomies of the calf for exertional compartment syndrome
Tibial intramedullary nailing (suprapatella approach): Synthes Expert Tibial Nail.
Author: Ross Fawdington FRCS (Tr & Orth)
Institution: The Queen Elisabeth Hospital, Birmingham,UK.
Clinicians should seek clarification on whether any implant demonstrated is licensed for use in their own country.
In the USA contact: fda.gov
In the UK contact: gov.uk
In the EU contact: ema.europa.eu
Online learning is only available to subscribers.



















