Schwannoma of the proximal radial nerve: Excision using posterior approach to humerus
Overview
Subscribe to get full access to this operation and the extensive Bone & Soft Tissue Tumour Surgery Atlas.
Watch the overview
Learn the Schwannoma of the proximal radial nerve: Excision using posterior approach to humerus surgical technique with step by step instructions on OrthOracle. Our e-learning platform contains high resolution images and a certified CME of the Schwannoma of the proximal radial nerve: Excision using posterior approach to humerus surgical procedure.
Schwannomas are benign peripheral nerve sheath tumours. They are rare, but the true incidence is unknown because they frequently present as incidental findings on magnetic resonance imaging (MRI). When superficially located they may present as painful lumps with electrical sensory symptoms of pins and needles, tingling and pain when knocked. When they occur in deeply located nerves they may present with symptoms associated with nerve compression especially if the tumour is sited at anatomically tight space.
Schwannomas grow slowly and the nerve accommodates the growing tumour, with neurological symptoms developing when compression is critical or the tumour reaches a size that distorts and compresses otherwise normal fascicles within a peripheral nerve. The symptoms experienced are dependent on the type of nerve and its anatomical location. Most tumours fall into the benign category and are either Schwannoma or Neurofibroma subtypes. Most are solitary but both can present as multiple tumours in neurofibromatosis. Multiple Schwannomas are also a feature of the separate genetic condition Schwannomatosis in which strings of multiple tumours may arise from a single nerve trunk.
Excision is recommended when they cause neuropathic pain or when there is developing neurological deficit. Following excision superficial nerves may remain sensitive or tethered in scar tissue. There is also a small risk of permanent neurological deficit following excision. The risk is greater after previous biopsy, in large tumours and with recurrent tumours. The decision to operate is usually based on symptom profile, careful clinical examination and MRI features. Atypical tumours with indeterminate imaging should be referred to a specialist unit where there is a soft tissue sarcoma MDT and biopsy planned with review of histopathology prior to excision. Malignant nerve sheath tumours are extremely rare but require specialist management for excision and reconstruction where indicated. The margins for excision are greater for proven or suspected malignant tumours and the focus in such cases is on tumour clearance rather than functional preservation, the opposite objective to that for benign tumours.
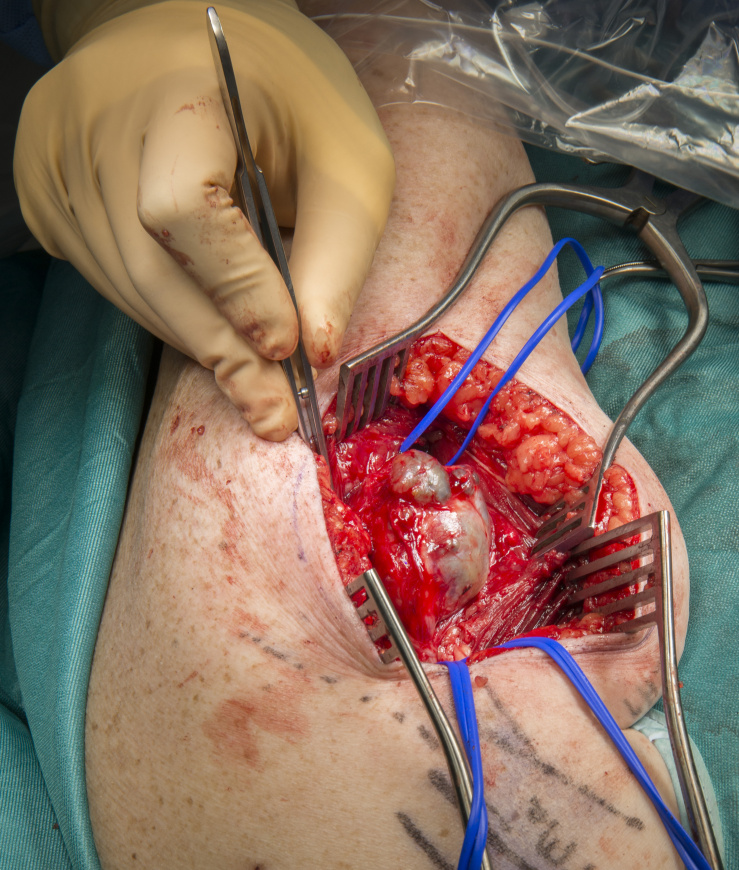
The case presented is a large Schwannoma in the radial nerve as it leaves the posterior axilla and extends into the spiral groove. The tumour was removed using a posterior approach to the humerus because of increasing size, pain, sensory symptoms and motor weakness. Prior to surgery the tumour had a biopsy and following this there was more pain, an increased tumour size and transient complete motor loss. Repeated imaging with MRI after the biopsy demonstrated a fluid level and suspected vascular malformation within the tumour.
Author: Dominic Power FRCS Tr & Orth, Consultant Hand and Peripheral Nerve Surgeon
Institution: Peripheral Nerve Injury Service, Birmingham Hand Centre, UK
Clinicians should seek clarification on whether any implant demonstrated is licensed for use in their own country.
In the USA contact: fda.gov
In the UK contact: gov.uk
In the EU contact: ema.europa.eu
Online learning is only available to subscribers.



















