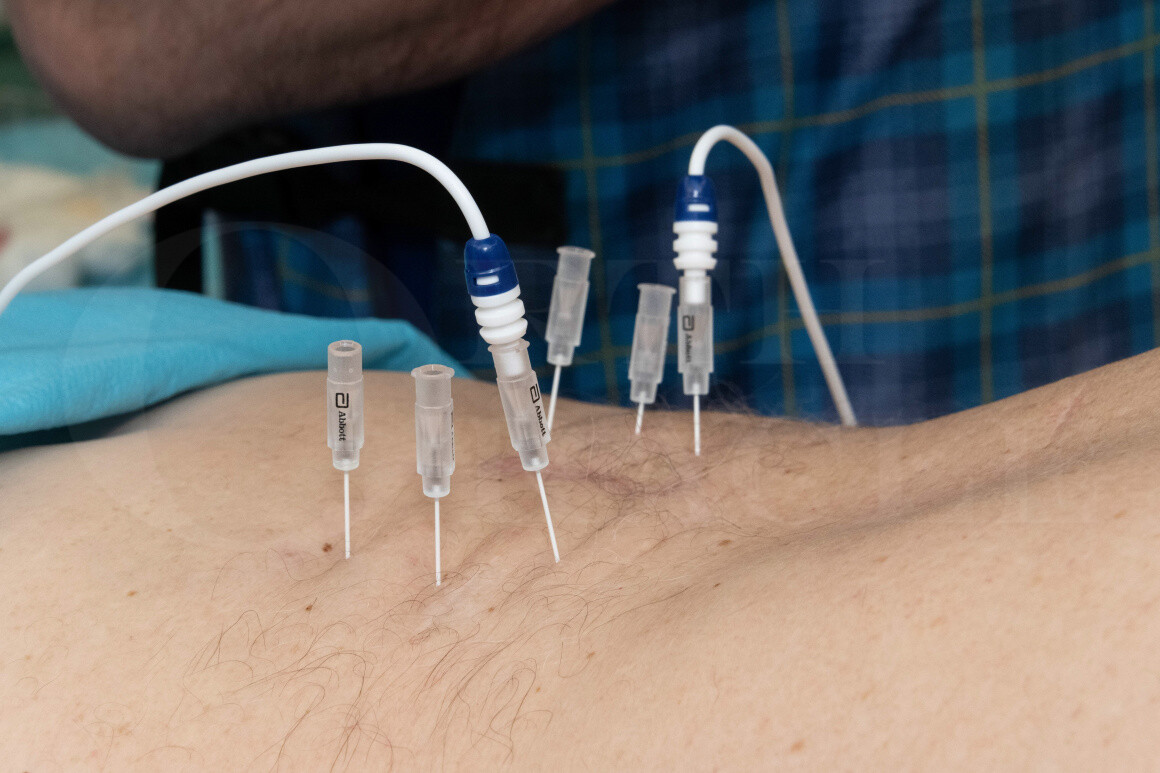
Facet Joint Denervation (lumbar spine) using Abbott IonicRF Generator
Overview
Subscribe to get full access to this operation and the extensive Spine Surgery Atlas.
Learn the Facet Joint Denervation (lumbar spine) using Abbott IonicRF Generator surgical technique with step by step instructions on OrthOracle. Our e-learning platform contains high resolution images and a certified CME of the Facet Joint Denervation (lumbar spine) using Abbott IonicRF Generator surgical procedure.
Lumbar spondylosis is a very common condition and is often seen as part of the normal ageing process of the spine. The term is used to describe degenerative changes seen in the spine, which include facet joint and disc degeneration. These changes may result in the development of back pain. If any of the degenerative changes cause compression of nerve roots, this can cause neuropathic radicular pain that presents as sciatica in the lower limbs.
Back pain related to degenerative changes is common and can normally be managed by optimising muscle function and staying active; physiotherapy input is useful to advise relevant core stability exercises and gluteal muscle strengthening to support the spine and standing alignment, and stretching exercises to prevent localised muscle spasm. However, ongoing back pain can cause progressive loss of function and inability to perform normal daily activities.
National guidance on the management of low back and radicular pain was released by NICE in 2016 (https://www.nice.org.uk/guidance/ng59). If patients have “red flags”, they should be referred for urgent imaging. Such “red flags” include night pain, being systemically unwell, progressive neurological deficit, progressive focal deformity, and ongoing pain resistant to conservative management. For patients who do not have red flags, the STarT Back tool can be used to plan which management pathway to follow; this was developed by Keele University to stratify severity of symptoms associated with low back pain and is commonly used in primary care and triaging services (https://startback.hfac.keele.ac.uk) to guide initial management. If there is no structural cause for the back pain, or there are many degenerative changes without a specific focal cause for the pain, this is classed as non-specific low back pain. For the management of non-specific low back pain, the best option is normally self-management and potentially a combined psychosocial and physical program if there is one available locally.
For patients with specific low back pain where there is a focal structural cause that correlates with the patient’s symptoms, options include injection therapy to identify pain sources and treat them. The effect of steroid injections only lasts for a short time so they are used in most patients to break the cycle of repetitive pain and muscle spasm, then allow them to continue with conservative measures; only rarely do patients require formal surgery. Steroid injections are most successful when used for an acute disc prolapse, since the prolapse often resolves by the time the steroid has worn off. However, other degenerative spinal pathology does not spontaneously improve over time, which is why patients need to be able to self-manage their symptoms or consider alternative treatment.
Low back pain can be due to the pain from the degenerative facet joints or degenerative disc disease. Traditionally, facet joint steroid injections were used for facet joint pain. This provided short term relief of pain originating from the joints but often wore off after a few weeks or months. Current guidance suggests aiming for treatments that provide a longer term relief of symptoms and facet joint denervation can be used for this. In order to confirm the pain is coming from the facet joint, a diagnostic local anaesthetic injection is placed around the medial branch sensory nerve of that spinal level, which will block sensation of pain from that facet joint. A small volume of local anaesthetic should be used to avoid anaesthetising other structures and adjacent levels (Wahezi SE et al, PM R 2018). If the diagnostic local anaesthetic ‘medial branch block’ reduces the pain, it is appropriate to proceed with a facet joint radiofrequency denervation. This can improve facet joint pain for two or three years but there is a chance that pain can return during that time. Most studies use a cutoff of >50% pain score reduction following medial branch block to consider proceeding with radiofrequency denervation, although it is worth considering that there may also be a confounding placebo effect. Medial branch block is likely to be a better prognostic indicator than intra-articular facet joint injection when examining the long term response to facet joint denervation (Cohen SP et al, Reg Anesth Pain Med 2015).
Radiofrequency denervation involves inserting a specialised needle under fluoroscopic or ultrasound guidance, so the tip lies next to the medial (dorsal) branch of the exiting nerve root at the medial dorsal aspect of the lumbar vertebra transverse process. One cannot see the nerve on imaging so the position of the nerve is presumed based on anatomical studies and a positive previous medial branch block. A probe is then inserted into that needle and a current is passed through the needle to coagulate the tissues around the tip of the needle. This disrupts the sensory supply to the facet joints and aims to remove the sensation of pain from that joint. It does not take away the underlying degenerative changes and the pain often returns with two or three years.
There are a number of different companies who have designed radiofrequency denervation equipment. I use the Abbott Neurotherm equipment in this technique since it utilises smaller diameter needles than other equipment (which produces less post-operative pain) and allows surgeon preferences to be saved for ease of process during the procedure.
OrthOracle readers will find the following associated instructional techniques of interest:
L5/S1 Anterior Interbody Lumbar Fusion [Globus INDEPENDENCE MIS®]
Midline Lumbar Spine decompression (for spinal stenosis)
Author: Mr Stephen Morris FRCS (Tr & Orth).
Institution: Avon Orthopaedic Centre, Southmead Hospital, Bristol
Clinicians should seek clarification on whether any implant demonstrated is licensed for use in their own country.
In the USA contact: fda.gov
In the UK contact: gov.uk
In the EU contact: ema.europa.eu



















