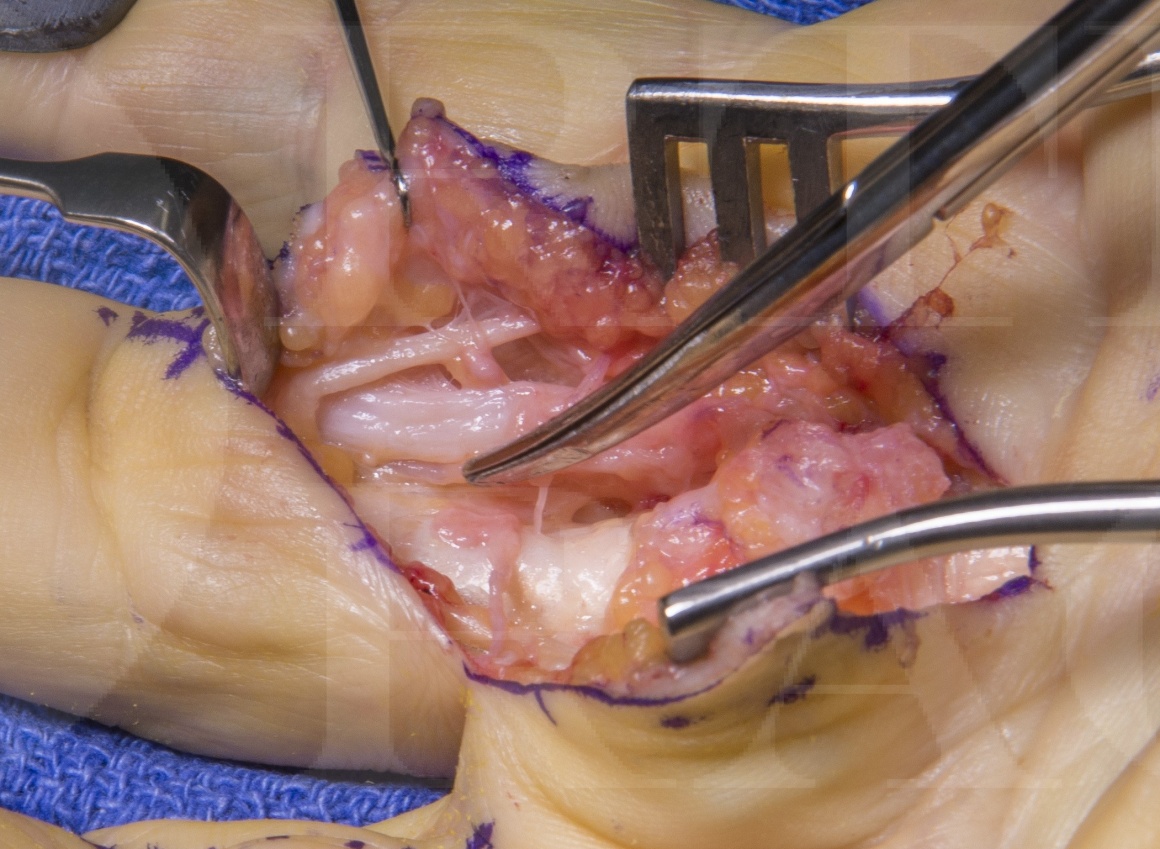
Dupuytrens contracture: Palmar and digital fasciectomy
Overview
Subscribe to get full access to this operation and the extensive Upper Limb & Hand Surgery Atlas.
Learn the Dupuytrens contracture: Palmar and digital fasciectomy surgical technique with step by step instructions on OrthOracle. Our e-learning platform contains high resolution images and a certified CME of the Dupuytrens contracture: Palmar and digital fasciectomy surgical procedure.
This is a detailed step by step instruction through one method of fasciectomy for Dupuytren’s contracture.
Dupuytren’s contracture is a relatively common condition which causes a histological alteration in a number of fascial structures within the palmar surface of the hand.
It is a clinical diagnosis and only rarely when there is a single nodule which has not caused any contracture in the early stages can it be difficult to diagnose.
75% of cases occur in the ulna 2 digits.
There is no current cure for the disease however there are 4 main groups of treatment options to improve contractures. These options are needle fasciotomy, fasciectomy, dermo-fasciectomy and collagenase injections. Within the fasciectomy group terminology becomes confusing with many terms being used synonymously despite original descriptions differing. Examples are focal, segmental and limited fasciectomy. There is also variation in a dermo-fasciectomy with a small fire-break skin grafts or a larger graft covering a clear anatomical section e.g. volar finger between MCPJ and PIPJ creases.
In addition, adjuncts to surgery such as temporary external fixators or salvage options such as amputation or joint arthrodesis are also included in the Dupuytren’s treatment armamentarium.
Fasciectomy, to be shown in this case can be performed under local, regional or general anaesthetic dependant on the disease pattern and anaesthetic support. The procedure is performed under tourniquet control and a patient normally is treated in plaster cast until their 1 week review where they start mobilisation and 3 months night splinting with the hand therapists.
Complications include failure of complete correction (common with severe PIPJ disease where the joint capsule and ligaments are contracted), recurrence (very common eventually with rates of 10-50% at 5 years depending on disease severity, joint involved and treatment method used), neurovascular injury (rare however increasing common the greater the number of revision surgeries at a single site), infection and stiffness. Graft failure in dermo-fasciectomy and allergy to collagenase are additional complications that are an additional risk with other methods mentioned.
Author: Mr Mark Brewster FRCS (Tr & Orth)
Institution: The Royal Orthopaedic Hospital, Birmingham, UK.
Clinicians should seek clarification on whether any implant demonstrated is licensed for use in their own country.
In the USA contact: fda.gov
In the UK contact: gov.uk
In the EU contact: ema.europa.eu
Online learning is only available to subscribers.



















