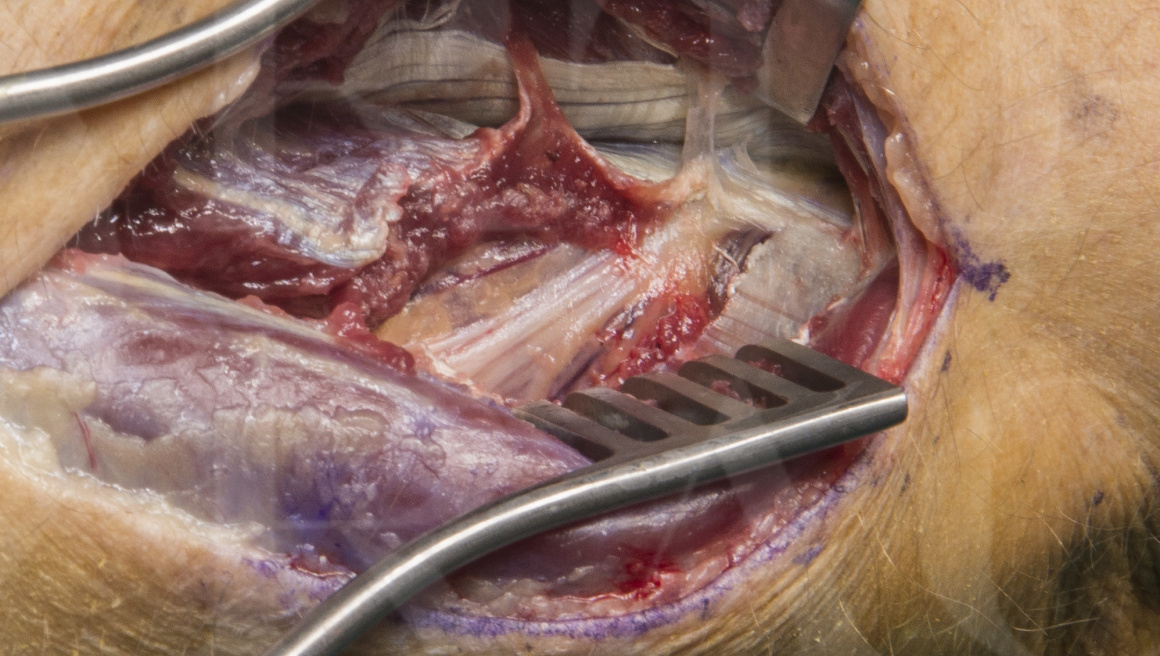
Posterior interosseous nerve decompression
Overview
Subscribe to get full access to this operation and the extensive Upper Limb & Hand Surgery Atlas.
Learn the Posterior interosseous nerve decompression surgical technique with step by step instructions on OrthOracle. Our e-learning platform contains high resolution images and a certified CME of the Posterior interosseous nerve decompression surgical procedure.
The posterior interosseous nerve (PIN) is a terminal branch of the radial nerve and supplies innervation to the extensor carp ulnaris (ECU) and the digital extensors. The PIN passes through the supinator tunnel to enter the dorsal forearm. The supinator tunnel is formed by the two heads of the supinator. The superficial head of supinator arises from the lateral epicondyle of the humerus and the deep head from the supinator crest of proximal ulna. The two muscle heads converge as they encircle the proximal radius and they form a common tendon that inserts to the radius shaft distal to the bicipital tuberosity. The nerve passes between the two heads. The PIN is in contact with the bone of the radius neck, but the deep head separates if from the radius shaft within the mid and distal thirds of the supinator tunnel. If the nerve is entrapped in the supinator tunnel patients present with dorsal forearm pain, worse with activity, limited digit extension and radial deviation of the wrist due to loss of the ECU’s stabilising effect on the pull of the extensor carpi radialis longus.
The common sites of entrapment are the leash of Henry (radial recurrent vessels) and the arcade of Frohse (proximal fibrous brach of the supinator). The nerve branches within the tunnel and at the distal end, as it emerges in the dorsal forearm it lies in close proximity with the posterior interosseous artery and gives branches to the ECU, EDC and EDM muscles. The remaining PIN passes distally and provides branches to the APL, EPB, EPL and finally the EIP muscles.
The nerve should be imaged in the tunnel to exclude intrinsic nerve tumours or extrinsic causes of nerve compression. The condition may be associated with proximal radio-capitellar synovitis and can also be of spontaneous onset with a viral inflammatory aetiology.
Decompression o the PIN in the tunnel may prevent further deterioration and salvage residual function in the posterior interosseous nerve, preventing further loss of digit extension.
The case illustrated had spontaneous onset of proximal dorsal forearm pain and loss of finger extension with normal imaging studies of the neck and he posterior interosseous nerve. Clinical examination demonstrated weakness in the PIN innervated muscles at MRC grade 2 that had persisted without recovery for three months. There was proximal tenderness over the proximal supinator and the PIN dorsally. Electromyography demonstrated partial chronic denervation of the PIN innervated muscles with intact function of the flexor carpi unlearns, suggestive of pathology at the level of the PIN and not more proximally at the C8 nerve root.
Author: Dominic Power MA MB BChir(Cantab), FRCSEd, FRCSLon, FRCS(Tr & Orth) Consultant Hand and Peripheral Nerve Surgeon, Honorary Senior Clinical Lecturer, University of Birmingham, UK.
Institution: West Midlands Peripheral Nerve Injury Service, Birmingham Hand Centre, UK
Clinicians should seek clarification on whether any implant demonstrated is licensed for use in their own country.
In the USA contact: fda.gov
In the UK contact: gov.uk
In the EU contact: ema.europa.eu



















