Revision Lumbar Microdiscectomy
Overview
Subscribe to get full access to this operation and the extensive Spine Surgery Atlas.
Learn the Revision Lumbar Microdiscectomy surgical technique with step by step instructions on OrthOracle. Our e-learning platform contains high resolution images and a certified CME of the Revision Lumbar Microdiscectomy surgical procedure.
Lumbar disc prolapse is a common condition which can cause lumbar nerve root compression and result in lower limb radiculopathy, a term that describes the symptoms produced by compression of a nerve root.
Everyone develops degenerative disc disease over the course of their life, with the lower lumbar discs generally being affected earlier than the upper lumbar discs. The vast majority develop a degenerative, broad based bulge that does not cause any neural compression. However, some people will develop a focal prolapse, or herniation, which can cause nerve compression. The most common location for a disc herniation is paracentral which is located within the spinal canal and causes compression of the traversing nerve root in the lateral recess. Less common locations for disc herniation include central, foraminal, and far lateral.
The incidence of lumbar disc herniation is between 0.5% and 2% and is most common in people in their fourth and fifth decades of life. It can sometimes be related to a specific incident involving heavy lifting or bending, but there is often no specific causative factor.
The lower limb radiculopathy caused by the neural compression can be severe and tends to be felt in the dermatomal area of the compressed nerve. The vast majority of disc prolapses do resolve spontaneously over time and this can generally take between 3 and 12 months. As such, most patients will be able to follow a non-operative course of treatment using analgesia and activity modification. Steroid injections around the nerve may help with pain relief during this time.
For those patients who cannot tolerate the pain despite non-operative measures or those who have a progressive neurological deficit, surgery may be beneficial.
Lumbar microdiscectomy is one of the most common spinal procedures performed and doctors managing spinal patients should be familiar with the management of lumbar disc herniation, the treatment options available, and the principles of a lumbar microdiscectomy.
Unfortunately, recurrence of the disc herniation can occur post-operatively in around 6% (range 5-24%) of patients undergoing lumbar discectomy. This has been found to be more common in patients who smoke, have diabetes mellitus, and who are obese. It most commonly occurs within three months of the primary surgery but may occur later than this.
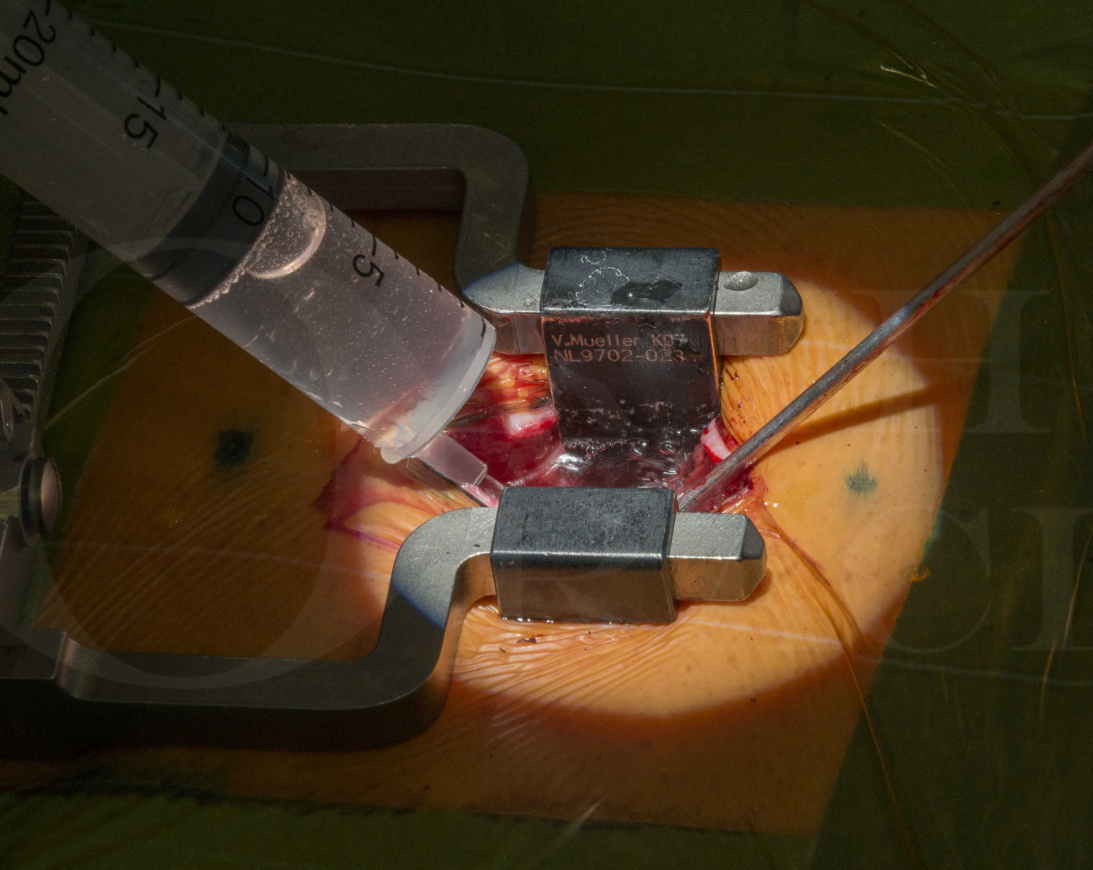
I routinely perform a microdiscectomy for primary cases as it provides excellent visualisation of the operative field whilst minimising peri-operative risks, and can often be performed as a daycase (out-patient) procedure. It can also be used for revision procedures due to the exposure created and allows excellent visualisation of relevant structures, particularly the nerves, dura, and scar tissue.
This technique describes the case of a patient who previously underwent a microdiscectomy and sustained a recurrent disc prolapse around six weeks post-operatively.
Readers will also find the following OrthOracle operative techniques of interest:
Lumbar microdiscectomy for cauda equina syndrome
Lumbar spine decompression for spinal stenosis
Thoracic discectomy (access by thoracotomy)
Anterior Cervical Discectomy and Fusion using the DePuy Zero-P VA cage
Author: Mr Stephen Morris FRCS (Tr & Orth).
Institution: Avon Orthopaedic Centre, Southmead Hospital, Bristol
Clinicians should seek clarification on whether any implant demonstrated is licensed for use in their own country.
In the USA contact: fda.gov
In the UK contact: gov.uk
In the EU contact: ema.europa.eu
Online learning is only available to subscribers.



















