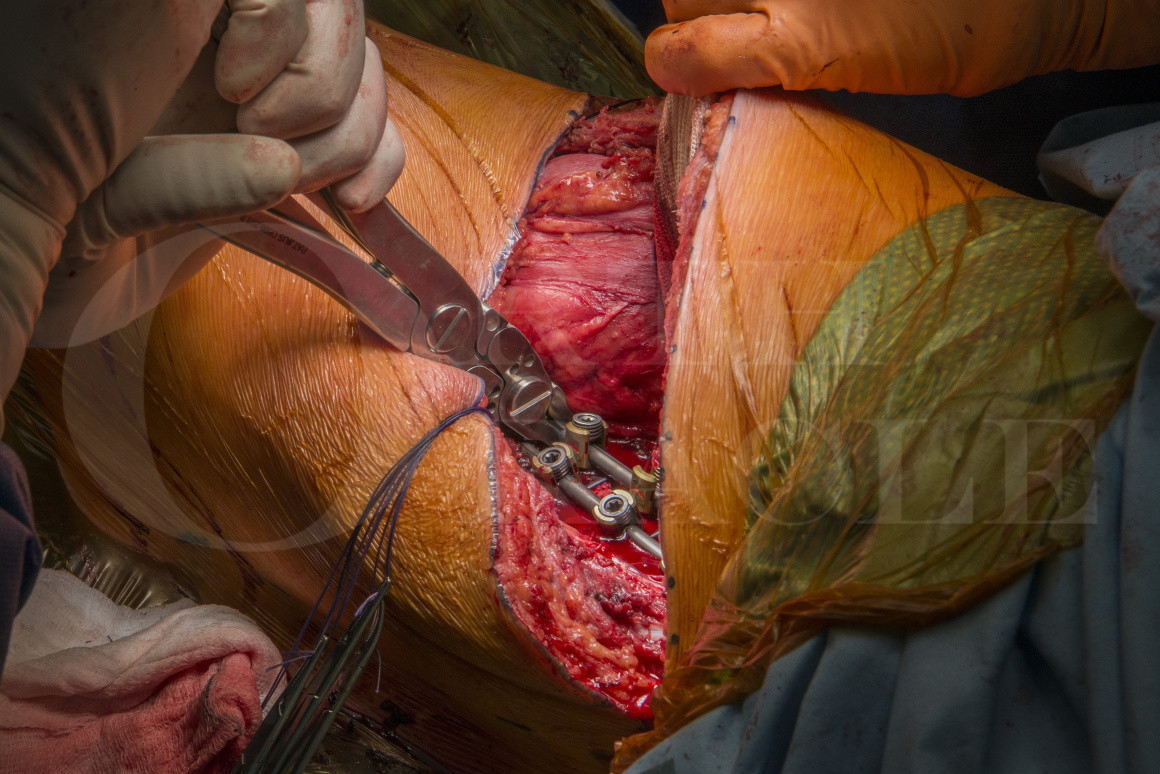
T11 to L3 anterior scoliosis correction and fusion with the Globus Anterior Staple System
Overview
Subscribe to get full access to this operation and the extensive Spine Surgery Atlas.
Learn the T11 to L3 anterior scoliosis correction and fusion with the Globus Anterior Staple System surgical technique with step by step instructions on OrthOracle. Our e-learning platform contains high resolution images and a certified CME of the T11 to L3 anterior scoliosis correction and fusion with the Globus Anterior Staple System surgical procedure.
Adolescent idiopathic scoliosis (AIS) is a complex condition of unknown aetiology and is the most common developmental spine condition in adolescents.
A scoliosis, by definition, is a lateral curvature of the spine of coronal Cobb angle of greater than 10 degrees. A scoliosis can develop secondary to congenital, syndromic, traumatic, pathological or neurologic conditions. In adolescents where no other aetiology is found, it is classified as an idiopathic scoliosis. Adolescent Idiopathic scoliosis is the most common form of scoliosis.
The term “idiopathic” to some extent is a mis-nomer as it suggests the aetiology is unknown whereas in truth it is simply not yet fully understood. Although AIS does not seem to be associated with any particular condition and is generally seen in otherwise healthy adolescents, research to date shows it to be a complex condition in which genetic, mechanical and hormonal factors are implicated in the pathogenesis.
Scoliosis develops in approximately 3% of children younger than 16 years but only 0.3-0.5% have progressive curves requiring treatment.
Presentation is usually between ages 10 to 18 years of age. Female to male ratio 1:1 for small curves; 10:1 for curves greater than 30 degrees. It encompasses a range of severity and is relatively common. In its milder forms, scoliosis may produce isolated trunk asymmetry. Very large curves, greater than 100 degrees, may cause severe disfigurement and, occasionally cardiopulmonary compromise.
Using a coronal Cobb angle to define a scoliosis deformity does somewhat over simplify the spinal deformities associated with the clinical presentation. The definition describes the spinal curve only in 2-Dimensions (10 degree lateral curvature) but a scoliosis is a 3-Dimension deformity. In addition to the coronal spine curvature there is segmental vertebral rotation (which creates a “spiral shape” rather than the “S-shape”). Vertebral rotation in the thoracic spine clinically results in a thoracic rib hump and in the thoracolumbar/lumbar spine a loin hump.
Some curves can be judged low risk of progression and/or causing later problems. In such clinical presentations, observation is needed until skeletal maturity.
Smaller curves at presentation, judged to be at risk of progressing, can be managed with bracing with the aim to prevent curve progression to a magnitude that may cause later problems (<45-50 degrees at skeletal maturity).
In children and adolescents, surgery is considered if the curve reaches a magnitude that could cause problems in adulthood (>50 degrees at the end of skeletal maturity). This Cobb angle “number” however is not (and should not be) binary; as in 50 degrees means no operation and 51 degrees means operation. I have many patients with curves greater than 50 degrees in whom the scoliosis causes no problems or concerns for the patient, and they lead very active lives. Patient and clinician in such circumstances discuss the benefit vs risk (immediate, medium and long term risks/consequences of instrumented scoliosis correction surgery) and a decision can be made by the patient for no intervention.
The goal of surgical treatment in AIS is to achieve and maintain a long term improvement in coronal deformity, sagittal balance and axial de-rotation while minimising the number of vertebral segments fused.
Operative management of scoliosis has progressed significantly over the past three decades. Posterior approaches have become the gold standard for treating majority of AIS curves since Harrington’s first report in the 1960s.
Controversy remains about the best approach to the management of thoracolumbar/Lumbar curves. The comparison between posterior instrumentation using pedicle screws and anterior approach using thoracolumbar and lumbar correction systems has been debated for years.
Proponents for anterior instrumented correction and fusion advocate the technique spares posterior musculature and attains good coronal correction with fusion of fewer distal motion segments.
Supporters of posterior approach express concern about potential morbidity of anterior instrumentation and that it’s more technically demanding. They feel with modern posterior pedicle screw systems similar outcomes can be achieved by posterior approach surgery.
In this module the anterior approach to the thoraco-lumbar spine will be demonstrated with instrumentation from T11 to L3 using Globus REVERE® Anterior Staple System.
The REVERE® Anterior Staple System is a dual (or single rod) staple system. All single and duel staples accommodate 5.5mm, 6.5mm and 7.5mm monoaxial screws.
Author: Neil Upadhyay FRCS (Tr & Orth)
Institution: The Avon Orthopaedic centre, Southmead Hospital, Bristol, UK.
Clinicians should seek clarification on whether any implant demonstrated is licensed for use in their own country.
In the USA contact: fda.gov
In the UK contact: gov.uk
In the EU contact: ema.europa.eu
Online learning is only available to subscribers.