Thoracic spine fracture dislocation: Posterior open reduction and instrumented fusion (Navigated Medtronic Solera 55/60 instrumentation)
Overview
Subscribe to get full access to this operation and the extensive Spine Surgery Atlas.
Learn the Thoracic spine fracture dislocation: Posterior open reduction and instrumented fusion (Navigated Medtronic Solera 55/60 instrumentation) surgical technique with step by step instructions on OrthOracle. Our e-learning platform contains high resolution images and a certified CME of the Thoracic spine fracture dislocation: Posterior open reduction and instrumented fusion (Navigated Medtronic Solera 55/60 instrumentation) surgical procedure.
Thoracolumbar fracture-dislocations follow high energy trauma and are inherently unstable. They involve injury to the bony and ligamentous structures that stabilize the spine and are often accompanied by a neurological injury (50-60% associated with spinal cord injury).
Overall, spine fractures account for 6% of all fractures worldwide. The reported annual incidence rates vary from 19 to 88 per 100,000 persons for spinal fractures. Usually result from motor vehicle accidents, falls, sports and violence.
Approximately 75% to 90% of spinal fractures occur in the thoracic and lumbar spine, with most of these occurring at the thoracolumbar junction (>50% at T10-L2).
Historically, treatment of spine trauma has been variable and based on anecdotal rather than systems-based practices with institutional, regional, and individual surgeon preferences often dictating management. Perhaps one of the principal reasons for such variability maybe because of a lack of an universally accepted classification system.
Between 1949 to present day, several classification systems have been proposed for spine trauma; these were based on retrospective reviews and the experience of individual surgeons: Nicoll (1949) described fractures and dislocations of the thoracolumbar spine based on risk of subsequent deformity and cord injury sustained from functional activity; Kelley and Whitesides (1969) proposed a biomechanical concept for stability which included anterior and posterior column support; Holdsworths (1970) proposed the posterior ligamentous complex was the sole key to spinal stability; and Denis (1983) expanded this to include a 3-column model which subsequently became popular but because many of these systems are convoluted, with an impractical number of variables or too simple and lacking sufficient detail to provide clinically relevant information none of the above classifications fully described the spinal injury and thus comprehensively aided decision making for their management.
In 2013, the AOSpine Knowledge Forum developed a spinal trauma classification system designed to be comprehensive. This is the classification system I use when communicating and deciding on management of spinal fractures. [Schnake, K. J, Dvorak, M. F, Benneker, L. M, et al. AO Spine-Spine Trauma Classification System: The Value of Modifiers: A Narrative Review With Commentary on Evolving Descriptive Principles. Global spine journal 2019; 9: 77S – 88S].
Introduced by the Spine Trauma Study Group in 2005, the TLICS (thoracolumbar injury classification and severity score) was designed to provide a clear, reliable classification system that accounts for many of the shortcomings of prior systems. Three major injury characteristics were defined: injury morphology, neurologic status, and integrity of the PLC. Point values are assigned to each major category based on injury severity. The sum of these points represents the TLICS severity score, which may be used to guide treatment [Vaccaro AR, Lehman RA Jr, Hurlbert RJ, et al. A new classification of thoracolumbar injuries: the importance of injury morphology, the integrity of the posterior ligamentous complex, and neurologic status. Spine 2005; 30: 2325 -2333].
Spinal stabilisation with internal fixation is indicated in unstable spinal fractures, spinal cord compression and progressive neurological deficit.
That said, even when one decides fixation of the spinal fracture is required, the optimal management for thoracolumbar fracture-dislocations remain controversial in that several techniques have been proposed ranging from long posterior instrumented fixation to shorter posterior instrumented constructs including either transforaminal thoracic interbody fusion or combined postero-anterior fusion. No single method has been established as the most superior with respect to the clinical outcome.
Posterior-Anterior (360) fusions, although from a radiological outcome may be considered “gold standard”, do have an associated morbidity from the anterior approach via lateral thoracotomy; particularly given these patients will typically have rib and sternal fractures.
The optimal timing for spinal stabilization plus or minus neuronal decompression also remains controversial but most centers would aim to surgically reduce and instrument unstable spine fractures within 24 hours of injury [Vallier HA, Super DM, Moore TA et al. Do Patients With Multiple System Injury Benefit From Early Fixation of Unstable Axial Fractures? The Effects of Timing of Surgery on Initial Hospital Course. Journal of Orthopaedic Trauma 2013: 27; 405 – 412].
Irrespective of treatments employed, spinal cord injured patients are at risk of skin problems due to include decubitus ulceration, venous thromboembolism, urosepsis (common cause of death), automic dysreflexia (potentially fatal), non-union, later deformity/post traumatic syringomyelia and major depressive disorder (11% patients with spinal cord injuries). Being able to mobilise and rehabilitate these patients early does reduces some of the afore mentioned risks.
Due to the nature and effects of spinal injuries, only 54% of all patients with spinal fractures return to their previous level of employment.
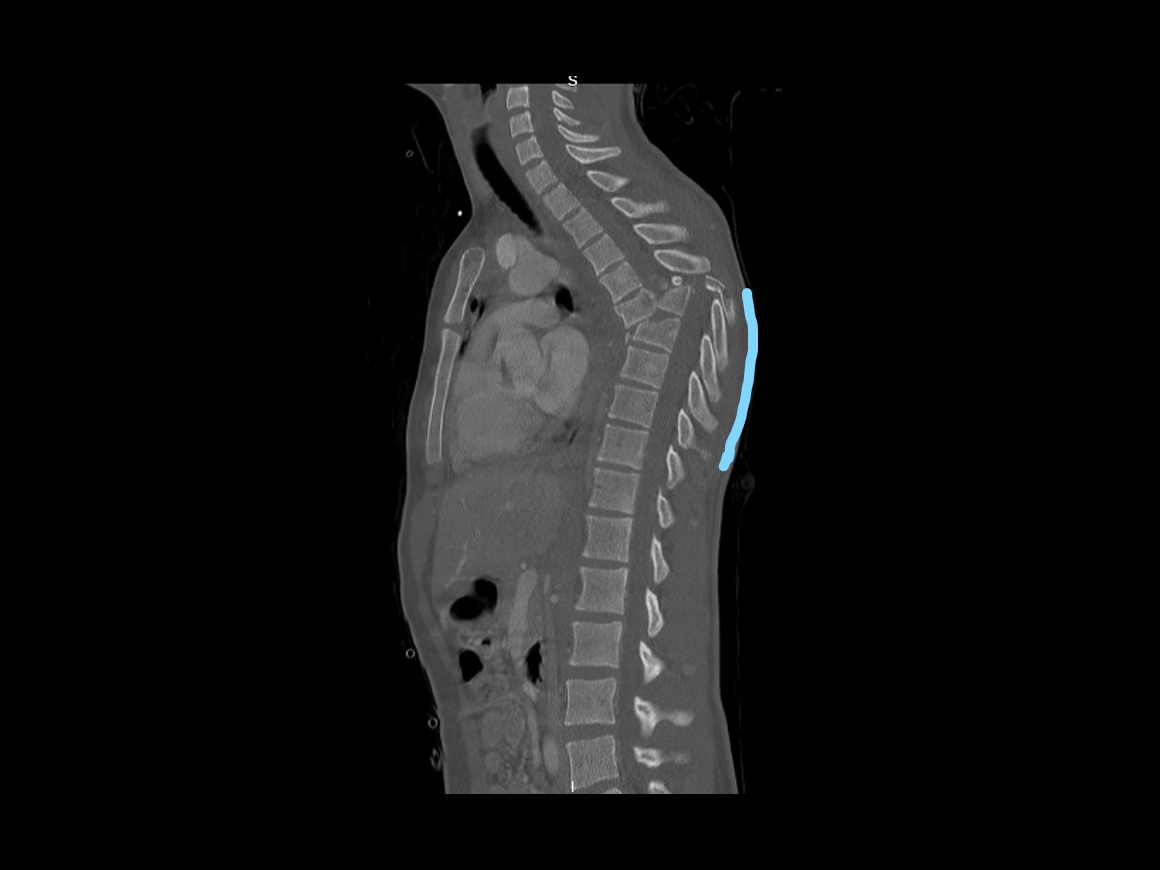
Here we present a case of an 18 year old who fell from significant height and sustained multiple injuries that included a T6/7 fracture dislocation with spinal cord transection and no distal neurological function distal to this level.
A T2 to T12 Navigated posterior instrumented fixation and fusion (following reduction of vertebral column) was performed using Medtronic Solera Instrumentation. Although several other implant options are available, having the option of intra-operative Navigation (Medtronic O-Arm and S8 Stealth station) at our hospital I believe helps in these more challenging cases. Often, in such significant high energy fractures, the normal anatomy is disrupted making use of normal landmarks to guide your instrumentation more difficult. Intra-operative image intensifier imaging can also be challenging to interpret when the spinal column is dislocated and overlapping. These aforementioned problems are not an issue with Navigation. The only problem with use the of Navigation in such unstable fractures is the surgeon must be aware of the risk for loss of intra-operative image referencing during the case. This occurs when movement of the spine occurs and the navigation system displays the anatomy where it was imaged and not where it currently maybe (after movement). For that reason, regular checking is needed and to perform at least two O-Arm spins (one spin to include the upper vertebral levels above the fracture and one spin to include the vertebral levels below the fractured level).
Readers will also find the following related OrthOracle instructional techniques of interest:
Author: Neil Upadhyay FRCS (Tr & Orth)
Institution: The Avon Orthopaedic centre, Southmead Hospital, Bristol, UK.
Clinicians should seek clarification on whether any implant demonstrated is licensed for use in their own country.
In the USA contact: fda.gov
In the UK contact: gov.uk
In the EU contact: ema.europa.eu
Online learning is only available to subscribers.



















