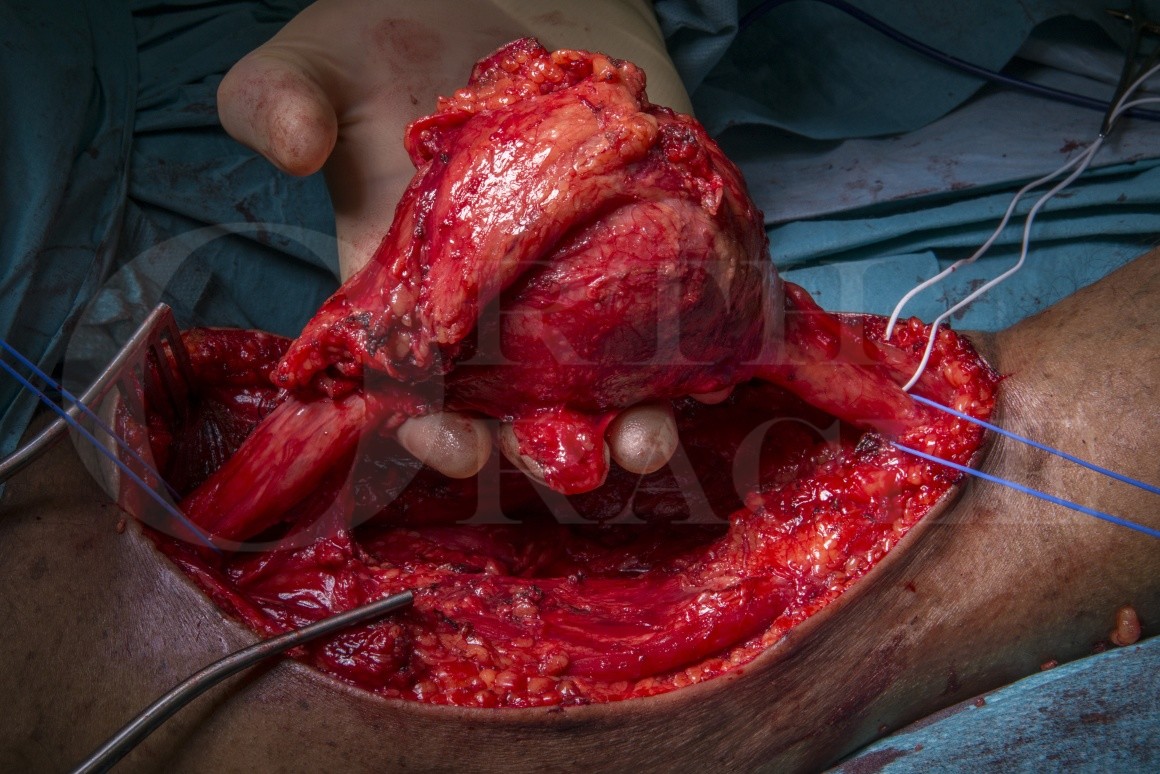
Sural nerve graft reconstruction of the sciatic nerve after resection of a malignant peripheral nerve sheath tumour
Overview
Subscribe to get full access to this operation and the extensive Upper Limb & Hand Surgery Atlas.
Learn the Sural nerve graft reconstruction of the sciatic nerve after resection of a malignant peripheral nerve sheath tumour surgical technique with step by step instructions on OrthOracle. Our e-learning platform contains high resolution images and a certified CME of the Sural nerve graft reconstruction of the sciatic nerve after resection of a malignant peripheral nerve sheath tumour surgical procedure.
Autologous reversed sural nerve cable grafting is the gold standard method for reconstruction of large nerve gaps in mixed (motor and sensory) major nerve trunks. Functional recovery is determined by the gap length, the site of the reconstruction, the duration of denervation, the surgical graft bed, the quality of the target muscles and the age of the patient. Malignant peripheral nerve sheath tumours (MPNST) are rare and usually present with a rapidly enlarging and painful mass with associated sensory and motor deficits. There may be a history of a neurofibromatosis which is associated with malignant transformation in peripheral nerve sheath tumours. Magnetic resonance imaging and biopsy are used to determine the diagnosis. The pathophysiological grade and the stage of disease determine the prognosis. Staging computed tomography will identify whether there are any metastases at presentation.
The surgical management involves excision of the tumour with a cuff of normal tissue to achieve an adequate surgical margin. Whilst the exact width of an adequate margin remains a sourc of constant debate, it should take into consideration the histological subtype, the quality of the margin tissue, the proximity of nearby vital structures and the use of adjuvant or neo adjuvant radiotherapy. In the case of large tumours and high grade histologies, compartment excision or ablative surgery may need to be considered to achieve an adequate margin. When post-operative radiation is required, non-vascularised autologous graft reconstruction is unlikely to support useful neural regeneration. In lower grade tumours, gap reconstruction with autologous graft provides a scaffold for nerve regeneration and results in less neuropathic pain, some proximal motor recovery and the chance of protective sensation to the plantar surface of the foot. Biopsy may lead to sampling error and the final grading of the tumour and adequacy of excision can only be determined on final specimen histopathological examination.
The case presented is a Malignant peripheral nerve sheath tumours that was biopsied and reported as low grade and surgical excise and bilateral autologous rural nerve cable grafting performed for gap reconstruction. The technique presented here will focus on the grafting technique and alternative options.
The tumour resection and discussion of the decision-making process for tumour management is covered in brief here but is covered in more detail with a technical description on OrthOracle at:
Excision of soft tissue Sarcoma ( thigh)
Author: Dominic Power FRCS (Tr & Orth) & Mike Parry FRCS (Tr & Orth)
Institution: Peripheral Nerve Injury Service & Royal Orthopaedic Hospital, Birmingham, UK
Clinicians should seek clarification on whether any implant demonstrated is licensed for use in their own country.
In the USA contact: fda.gov
In the UK contact: gov.uk
In the EU contact: ema.europa.eu
Online learning is only available to subscribers.



















