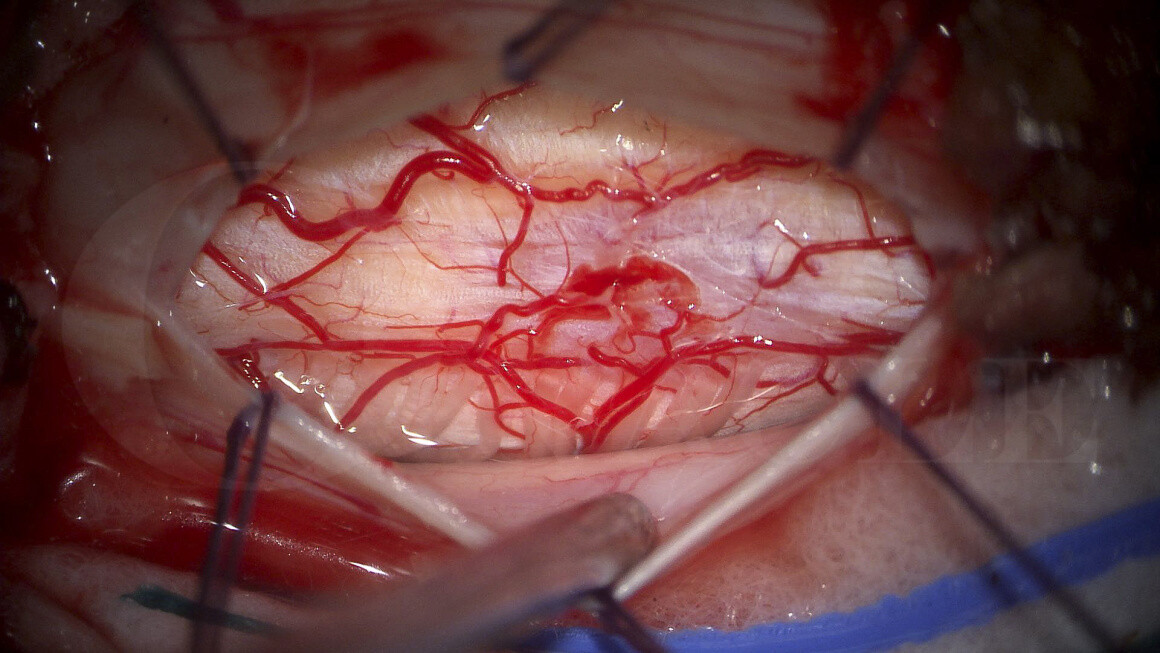
Cervical laminectomy and resection of spinal cord tumour
Overview
Subscribe to get full access to this operation and the extensive Spine Surgery Atlas.
Learn the Cervical laminectomy and resection of spinal cord tumour surgical technique with step by step instructions on OrthOracle. Our e-learning platform contains high resolution images and a certified CME of the Cervical laminectomy and resection of spinal cord tumour surgical procedure.
Intramedullary spinal cord tumours (IMSCT) are tumours that arise from the spinal cord. These tumours are rare and are very challenging to treat. The spinal cord is extremely eloquent neural tissue, meaning these tumours tend to cause spinal cord dysfunction and significant patient morbidity.
IMSCT comprise 20-30% of all primary intradural tumours. The other 70% are intradural extramedullary tumours (IDEM) that arise outside the spinal cord but inside the dura. This is an important distinction as IDEMs only cause extrinsic compression of the spinal cord, and treatment carries much less risk.
The most common IMSCTs are gliomas. These can be subdivided into astrocytomas (60-70%) and ependymomas (30-40%). Astrocytomas are locally aggressive and not normally amenable to complete surgical resection. Ependymomas tend to have a clear capsule and tumour-spinal cord interface and are therefore more amenable to complete resection.
The next most common are haemangioblastomas (15%), followed by rarer lesions that include germ cell tumours, haematopoietic tumours, lipomas and metastases. The differential diagnosis should also include other intrinsic pathologies to the spinal cord such as inflammatory lesions, trauma and infection.
It is usually not possible to be certain on the underlying diagnosis without histological confirmation. However, a neuroradiologist should be able to distinguish between an IMSCT and an IDEM.
Surgical treatment is usually the only means to make a definitive diagnosis of an IMSCT. This comes with a very high risk of causing worsening neurological deficit. This can range from a mild sensory deficit to a catastrophic spinal cord injury. Timing of treatment is therefore crucial, and needs to be tailored to the individual patient, taking into account their clinical status, rate of progression and psychosocial and lifestyle factors. Surgery is almost never required in an emergency setting. Pre-operative planning and thorough patient counselling are mandatory prior to surgery which should be done in a planned, elective manner.
Author: Mark Nowell FRCS
Institution: The Avon Orthopaedic Centre, Southmead Hospital, Bristol.
Clinicians should seek clarification on whether any implant demonstrated is licensed for use in their own country.
In the USA contact: fda.gov
In the UK contact: gov.uk
In the EU contact: ema.europa.eu
Online learning is only available to subscribers.



















