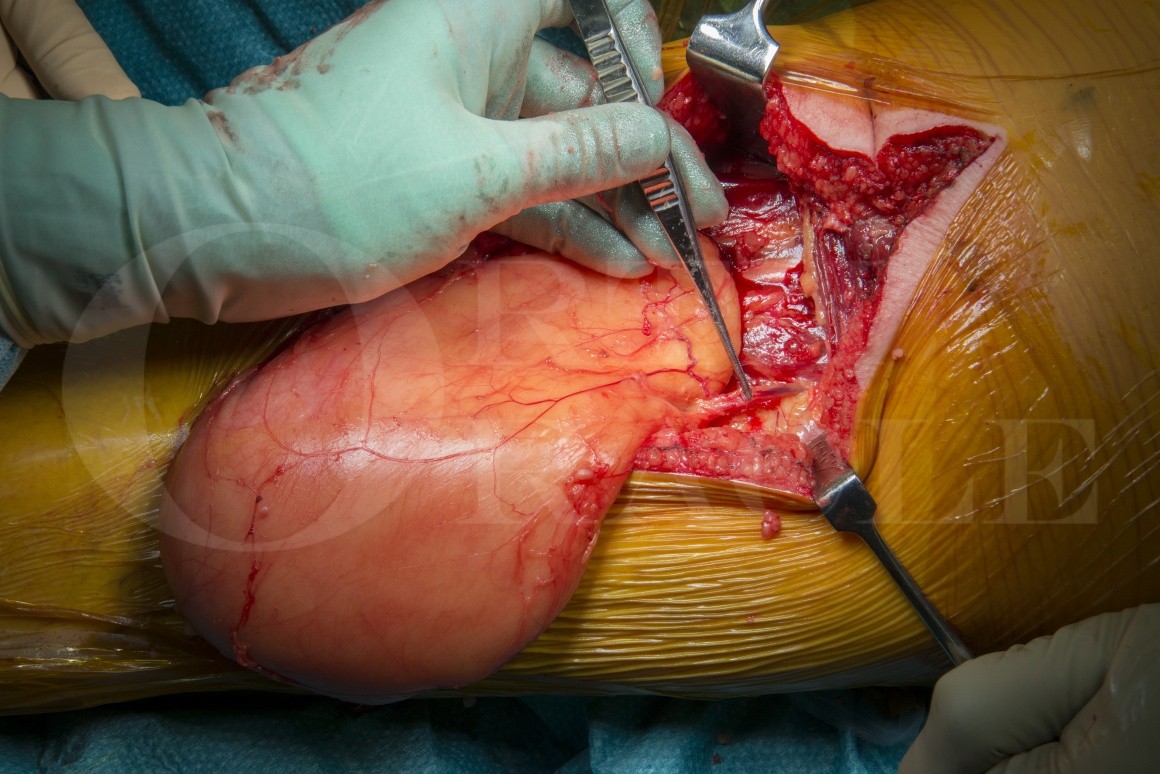
Excision of atypical lipomatous tumour from the posterior compartment of the thigh
Overview
Subscribe to get full access to this operation and the extensive Bone & Soft Tissue Tumour Surgery Atlas.
Learn the Excision of atypical lipomatous tumour from the posterior compartment of the thigh surgical technique with step by step instructions on OrthOracle. Our e-learning platform contains high resolution images and a certified CME of the Excision of atypical lipomatous tumour from the posterior compartment of the thigh surgical procedure.
Lipomatous tumours are the most common benign and malignant soft-tissue tumours encountered in clinical practice, typically presenting in middle to old age, but can occur in children and adolescents. Benign superficial lipomas classically arise in the subcutaneous tissue of the back, shoulder, neck and proximal extremities. Intra-muscular lipomas also occur and are found within or between muscles and adherent to joints, tendons, bone and nerves. In 5% of cases, lipomas can be multiple and symmetrical across the dorsum and proximal upper limbs.
Examination reveals solitary, soft, painless, mobile and slow growing lesions. Deeply located lipomas may be occult and therefore larger at presentation. Radiographs may reveal a radiolucent swelling, which appear as encapsulated, homogenous, high signal lesions on T1 with isointense signal to adjacent subcutaneous fat and fully suppress on fluid sensitive PD sequences. These are avascular lesions with no uptake with angiography, scintigraphy or contrast.
After marginal excision, these lobulated yellow tumours demonstrate mature adipoctyes organised in lobules with empty cytoplasm. Excision is curative and recurrences are rare in superficial lipomas, more common with intra-muscular lipomas.
Liposarcomas account for 10% of all soft-tissue sarcomas, and are the most common malignant soft-tissue sarcomas, typically arising in adults after the third decade. They can arise in any location with fat, but the majority are found deep to the facia in the thigh, groin, calf, popliteal fossa and buttock. These insidious lesions can reach large sizes prior to presentation and a few may have pain. Nerve compression or oedema secondary to venous occlusion can occur, particularly if involving the retroperitoneum. MRI sequences reveal heterogeneous and non-specific appearances of high and low signal regions on T2. These tumours can erode adjacent cortical bone which responds with a modest periosteal reaction. They show diffuse uptake with scintigraphy and angiography shows dense neo-angiogenesis.
Liposarcomas comprise a spectrum of low to high-grade lesions. Atypical lipomatous tumours (ALTs) are considered locally aggressive with histological features of cellular atypia (low grade) and may also be called ‘well differentiated lipoma like liposarcomas’ in other centres, although using the term ‘liposarcoma’ do describe a lesion that doesn’t metastasise is controversial and potentially upsetting for patients (https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1445-2197.2005.03519.x).
ALTs account for 40% of all liposarcomas, and have a recurrence rate of <10% with marginal excision. They are rarely lethal (unless arising in retroperitoneal or abdominal sites where they behave more aggressively). Differentiating lipomas from atypical lipomatous tumours is assisted using cytogenetic MDM2 amplification by fluorescence in situ hybridisation (FISH). In one study none of the benign lipomatous lesions demonstrated MDM2 amplified making this a valuable tool in the diagnosis of well-differentiated lipomatous neoplasms (Weaver J, Downs-Kelly E, Goldblum JR, et al. Fluorescence in situ hybridization for MDM2 gene amplification as a diagnostic tool in lipomatous neoplasms. Mod. Pathol.[Internet]. 21(8), 943–9 (2008). Available from: http://www.ncbi.nlm.nih.gov/pubmed/18500263.)
Authors: Robert Grimer & Jonathan Stevenson.
Institution: The Royal Orthopaedic Hospital, Birmingham, UK.
Clinicians should seek clarification on whether any implant demonstrated is licensed for use in their own country.
In the USA contact: fda.gov
In the UK contact: gov.uk
In the EU contact: ema.europa.eu
Online learning is only available to subscribers.



















