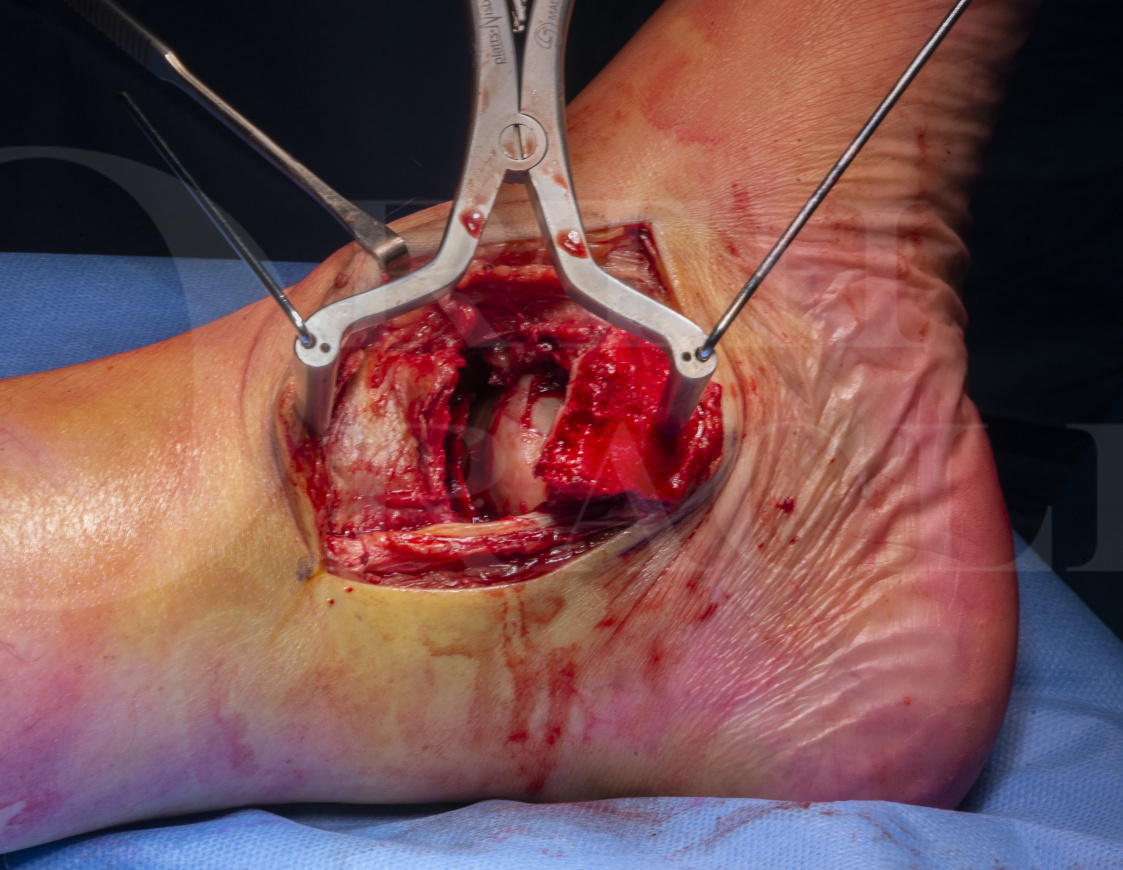
Talar fracture: Fixation of talar body and talar neck fractures via medial malleolar osteotomy
Overview
Subscribe to get full access to this operation and the extensive Foot Surgery Atlas.
Learn the Talar fracture: Fixation of talar body and talar neck fractures via medial malleolar osteotomy surgical technique with step by step instructions on OrthOracle. Our e-learning platform contains high resolution images and a certified CME of the Talar fracture: Fixation of talar body and talar neck fractures via medial malleolar osteotomy surgical procedure.
In general terms, fractures of the talus can be broadly divided into low and high energy injury patterns. Examples of low energy fractures include avulsions, osteochondral fractures and talar process fractures. High energy injuries will either lead to the relatively uncommon situation of talar extrusion or, more frequently, fracturing of the neck or body of the talus. In these instances, the talar fracture is often associated with other injuries that may need more urgent treatment, but equally a significant proportion of these injuries will need emergent care because they are open.
The mechanism of injury in talar neck fractures is forced ankle dorsiflexion in combination with forefoot supination. Body fractures often occur in a similar vein but have the additional element of axial loading and the hindfoot being in varus or valgus on impact. A fracture of the talar body is differentiated from a talar neck fracture by the presence of a primary coronal plane fracture line on the inferior surface of the talus involving the posterior facet of the subtalar joint. In reality, our experience in Sheffield is that invariably, body fractures also involve the neck of the talus.
It is well appreciated that both talar fracture types are associated with a poor outcome but the prognosis of displaced body fractures is uniformly poor, even when compared to talar neck fractures. It is really important not to lose sight of the fact that there are two reasons why this is the case. Firstly, the injury to the bone (and its vascular supply) and soft tissues. This has already occurred to the patient and cannot be undone. Therefore, the second reason for poor outcome is down to the further iatrogenic insult from the surgical treatment. As a surgeon, you have control of this latter cause. Therefore, careful planning is required before embarking on any surgery and this planning needs you to consider which of the key vessels that give the talus its notoriously poor blood supply have been compromised by the initial injury. Remember that 60% of the surface of the talus is covered in articular cartilage. The remaining forty per cent is occupied by joint capsular reflections and ligament insertions and that there are no tendon origins or insertions. The vascular supply to the talus arises from anastomoses from the anterior tibial artery (36%), the posterior tibial artery (47%) and the peroneal artery (17%) with relative contributions of flow indicated in brackets. Inferiorly, there is a significant supply from the anastomoses within the tarsal canal and medially through branches lying within the deep deltoid ligament.
In the following case, a 60 year-old male fell 10 feet from a ladder onto concrete. He sustained a closed injury to his left talar neck and body and the soft tissues were not threatened by any dislocated fracture fragments. This was an isolated injury.
Author: Mr Mark Davies FRCS Tr & Orth.
Institution: The Northern general Hospital, Sheffield, UK.
Clinicians should seek clarification on whether any implant demonstrated is licensed for use in their own country.
In the USA contact: fda.gov
In the UK contact: gov.uk
In the EU contact: ema.europa.eu
Online learning is only available to subscribers.