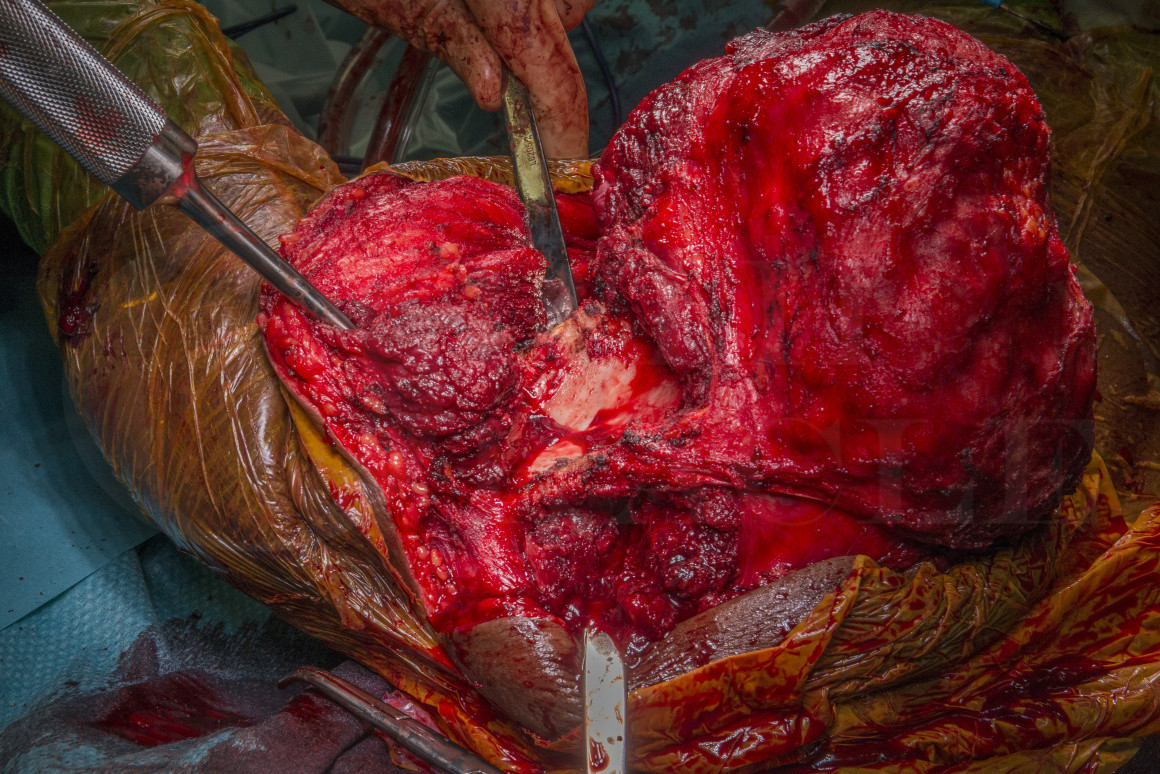
Partial scapulectomy: Chondrosarcoma
Overview
Subscribe to get full access to this operation and the extensive Bone & Soft Tissue Tumour Surgery Atlas.
Learn the Partial scapulectomy: Chondrosarcoma surgical technique with step by step instructions on OrthOracle. Our e-learning platform contains high resolution images and a certified CME of the Partial scapulectomy: Chondrosarcoma surgical procedure.
Osteochondromas represent approximately 1/3 of all benign bone tumours. They are an exostosis of bone that is covered by cartilage on its external surface. They typically present in the second or third decades of life and most frequently effect the appendicular skeleton, with the lower-limbs more commonly effected. They may be solitary or multiple hereditary osteochondromas. The risk of sarcomatous change is rare, seen in approximately 1% of solitary osteochondromas, with rates of 2-5% seen in hereditary multiple osteochrondromatosis (as in this case). Although classically osteochondromas are encountered in the metaphyseal region of appendicular long bones, axial tumours of the pelvis, spine, ribs, and scapula.
Surgery for benign osteochondromas should be avoided and only performed if they cause pain, decreased range of motion, pressure on neurovascular structures, tendon irritation or significant bursal formation. Clearly any clinical, pathological or radiological evidence of malignant transformation is also an indication for wide ‘en-bloc‘ resection of a possible chondrosarcoma.
In this case a young female patient suffered pain and limitation of movement as the osteochondroma continued to enlarge after skeletal maturity, a concerning feature of malignant transformation. An MRI pre-operatively had not excluded the possibility of malignant transformation and the biopsy was typically reassuring but subject to the sampling error renowned when biopsying possible chondrosarcomas. Unfortunately chondrosarcomas are not homogenous, and consequently high grade chondrosarcomas when carefully scrutinised after resection will have benign, low-grade and high-grade areas all within the same tumour, thus biopsy is considered unreliable. This has been reported by multiple research teams (Laitinen MK, Stevenson JD, Parry MC, Sumathi V, Grimer RJ, Jeys LM. The role of grade in local recurrence and the disease-specific survival in chondrosarcomas. Bone Joint J. 2018 May 1;100-B(5):662-666. doi: 10.1302/0301-620X.100B5.BJJ-2017-1243.R1. PMID: 29701096). The sarcoma MDT took the view that given the clinical and radiological features were concerning for sarcomatous transformation in a pre-existing osteochondroma, that en-bloc excision was indicated.
Malawer classified shoulder girdle resections for patients undergoing limb sparing procedures for bone and soft tissue tumours: Type I, proximal humeral resection; type II, partial scapular resection; type III, total scapulectomy; type IV, total scapulectomy and extra-articular glenohumeral resection; type V, proximal humeral and glenoid resection; and type VI, proximal humeral and total scapular resection. Here we present a type II partial scapulectomy for peripheral chondrosarcoma without reconstruction.
OrthOracle reader will find the following related operative techniques also of interest:
Forequarter amputation for chondrosarcoma
Hindquarter amputation with pedicled fillet flap for clear cell chondrosarcoma of the proximal femur
Proximal femoral endoprosthetic replacement (Stanmore METS, Stryker) for chondrosarcoma
Author: Jonathan Stevenson FRCS (Tr & Orth)
Institution: The Royal Orthopaedic Hospital, Birmingham, UK.
Clinicians should seek clarification on whether any implant demonstrated is licensed for use in their own country.
In the USA contact: fda.gov
In the UK contact: gov.uk
In the EU contact: ema.europa.eu



















