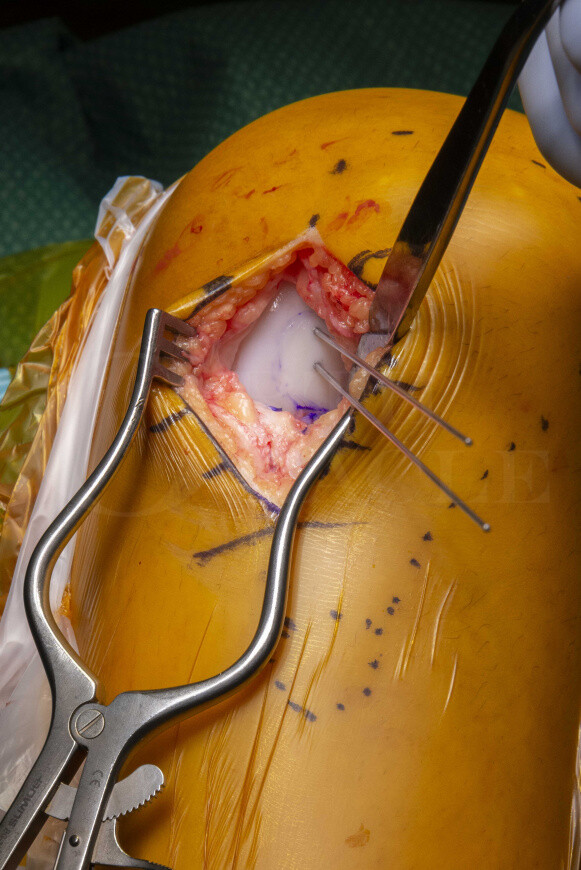
Osteochondral defect knee: Fixation(open) with Arthrex Biocompression screw
Overview
Subscribe to get full access to this operation and the extensive Knee Surgery Atlas.
Learn the Osteochondral defect knee: Fixation(open) with Arthrex Biocompression screw surgical technique with step by step instructions on OrthOracle. Our e-learning platform contains high resolution images and a certified CME of the Osteochondral defect knee: Fixation(open) with Arthrex Biocompression screw surgical procedure.
Chondral and osteochondral injuries are common. They typically affect the young, athletic population and can result in pain, mechanical symptoms and functional impairment. In the longer term the articular cartilage will likely lose its ability to adapt to repetitive stresses and osteoarthritis will ensue.
Articular cartilage is a thin layer of highly specialised connective tissue with complex viscoelastic properties. It is hypocellular, avascular and aneural with limited intrinsic healing capacity. It provides a smooth, lubricated surface for articulation and facilitates the transmission of loads to the underlying subchondral bone.
The avascularity is speculated to limit progenitor cell infiltration, which is necessary for cartilage regeneration. Adequate treatment of osteochondral defects (OCDs) is therefore essential to prevent progressive tissue loss and ultimately degenerative joint disease.
Osteochondral lesions of the knee may be secondary to trauma or osteochondritis dissecans. Traumatic injuries can be thought of as a spectrum of disease ranging from mild bone bruising to a focal chondral lesion to an osteochondral fracture. Osteochondritis dissecans is a not dissimilar phenomenon characterised by a separation of an osteochondral fragment from the articular surface. Approximately 75% of cases affect 10-20 year olds and they are twice as common in males compared to females. In 70% of cases the knee is affected and in 75% of these cases the medial femoral condyle is involved. The aetiology of osteochonditis dissecans is unclear and likely multifactorial: indirect or repetitive microtrauma is the most likely cause with persistent microstresses when the bone is growing interrupting the capsular blood supply leading to subchondral bone infarction.
The aim of treatment for both an osteochondral injury and osteochondritis dissecans is to preserve the native articular hyaline cartilage and promote healing of the osteochondral layer and subchondral bone. This is best achieved with anatomic reduction and internal fixation if the injury is relatively acute and / or has healing potential. If this is not possible or fixation has failed the mainstay of treatment consists of either some form of bone marrow stimulation in an effort to recruit mesenchymal stem cells and a fibrocartilaginous repair, or cartilage transplant with the hope of forming new hyaline-like cartilage.
Osteochondral fragments, flaps or grafts with sufficient bone stock are ideal for fixation with compression screws. In the more common medial femoral condyle defect this can be achieved arthroscopically using a lateral portal for visualisation and the medial portal for hardware placement. The procedure can also be performed via a mini-open approach (as in this case), which allows better visualisation and preparation of the fragment.
In cases where the lesion has an in situ fragment, the osteochondral lesion needs to be assessed for stability. The peripheral rim of the lesion needs to be stressed with a 5-mm arthroscopic probe. If the peripheral rim demonstrates impending instability (ie, cartilage fissure or breach at the periphery) but the cartilage lesion cannot be hinged open from the base/crater these lesions can be fixed in situ. Unstable lesions where the osteochondral fragment can be hinged open and the underlying subchondral bone visualised, or where a loose fragment has become separated from its base, require preparation of the bone at the base of the lesion to expose a bleeding cancellous bed. This can be achieved with burrs, osteotomes, Chondro Picks, curettes, or a 2 mm drill bit.
The Arthrex bio-compression screws used in this case are designed with a stepped pitch and taper, which draws the two fragments together using straightforward instrumentation. They are made of solid enhanced PLLA (poly-L-lactic acid) which absorbs over time without losing strength during the healing phase. I favour the Arthrex kit as it has straight forward instrumentation, provides good compression and if necessary the fixation can be augmented with darts or other fixation devices from the same manufacturer.
With anatomical reduction and satisfactory fixation most patients should expect normal function and remain largely asymptomatic. There are a number of studies confirming this in the medium-term (5 to 10 years). In the longer-term, however, there are only a handful of studies in the literature, but most suggest a good outcome regardless of skeletal maturity, the size and the severity of OCD lesion if fixation is anatomical and healing has occurred.
OrthOracle readers will also find the following associated instructional techniques of interest:
Stem cell harvest and transplant for knee osteochondral defect (Synergy Medical technologies)
Femoral trochlea chondral lesion: Chondrogide membrane(Geistlich pharma) for chondral regeneration.
Medial Femoral Condyle Focal Resurfacing with HemiCAP(Arthrosurface)
Stem cell harvest and transplant for knee osteochondral defect (Synergy Medical technologies)
Osteochondral grafting of the talus (OATS procedure)
Author: James Donaldson FRCS (Tr & Orth)
Institution: The Royal national orthopaedic hospital, Stanmore, London, UK.
Clinicians should seek clarification on whether any implant demonstrated is licensed for use in their own country.
In the USA contact: fda.gov
In the UK contact: gov.uk
In the EU contact: ema.europa.eu



















